Plastic & Reconstructive Eyelid Surgery
General Overview:
The eyelids are small but delicate structures essential for maintaining the health of the eyes and for protecting the eye. As we age, the skin thins out, tissue stretches and sags and the soft tissue loses volume. Heavy upper eyelids (ptosis) may interfere with vision. Loss of elasticity of the skin and sagging, baggy eyelids may take place.
Eyelid reconstruction may be undertaken in a variety of situations. Defects in the eyelid may originate from a variety of situations, but most commonly after trauma or tumor excision ( ). Simple superficial defects in the eyelid may occur after minor trauma or removal of small growths. Many of these require nothing more than local wound care and will heal on their own in a week to 10 days. Some simple superficial defects may require a few sutures (eyelid suturing), with the same local wound care.
In some cases, such as after traumatic eyelid injuries or removal of larger growths or skin cancers, larger defects may involve the entire lid. Many of these can be sutured together directly (edge to edge eyelid suturing), but many others may require even complex eyelid reconstructions. In many of these more complex cases, the surgeon will need to use transfer of adjacent tissues (“flaps”), or transfer of skin from other parts of the eyelid face or body (“skin grafts”) to complete the reconstruction. Some of these more complex reconstructions may require more than one operation to complete (“staged eyelid reconstruction”).
The goal of functional or reconstructive eyelid surgery is to refine abnormal function, remodel deformities, recondition defects due to tumour or tumour ablative surgery and in general to restore regularity/normalcy of the eyelid.
Reconstructive Eyelid Surgery can treat the following ocular conditions:
- Entropion
- Ectropion
- Ptosis
- Eyelid retraction
- Eyelid malpositions
- Blepharophimosis
- Eyelid synkineses
- Blepharospasm
- Eyelid tumours – such as and
Listed below are the different oculoplastic eyelid reconstructive procedures, used post eyelid cancers & defects:
Eyelid Tumours: Basal cell carcinoma of eyelid & other Nonmelanoma cancers of skin are predominantly seen in the eyelid region. These type of skin cancers are relatively unlikely to spread to the adjacent lymph nodes and distant sites (metastasis), but with eyelid skin cancers there is a significant risk for tissue damage to nearby vital structures of the eye and may even lead to blindness; the skin around the eyelid is thin and comprises of little subcutaneous tissue. The anatomical connections to the bone underlying the region help in spreading the tumor locally into the cavities behind the eyes & the nose. Skin cancer needs to be removed surgically.
Mohs Surgery: Removing a layer of skin and examining it immediately under a microscope, then removing many layers of skin until there are no signs of the cancer; generally used for skin cancers on the nose, ears, and other areas of the face. Mohs surgery ensures that post surgery, the chances of recurrence are limited, as the adjacent areas are examined for being ‘cancer free’ during surgery itself. Mohs microscopic surgery also ensures that more amount of health tissue post removal of skin lesions can be preserved.
Reconstruction of eyelid defects after tumor excision should aim at obtaining full globe protection, without visual disruption and restoring the area to an appearance as close to normal as possible. Reconstruction of the eyelids requires special considerations and complete understanding of the specialized anatomy of the region. The eyelids consist of an anterior lamella of skin, orbicularis muscle; posterior lamella of tarsus and conjunctiva. Full thickness defects of eyelid after tumor resection require reconstruction of these layers. However reconstruction of the skin and subcutaneous tissue can be easily reconstructed with skin grafts and local flaps, most important subject is reconstruction of the posterior lamellar segment of the eyelid. Tarsal plate is dense, fibrous tissue (not a cartilage!) that gives the eyelid its contour and provides its skeleton. Tarsal substitutes including banked sclera, nasal cartilage, ear cartilage, and periosteum can be beneficial for posterior lamellar repair. Reconstruction of the conjunctiva is more complex issue. Reconstructive plastic surgery eyelid techniques can be classified considering the anatomical area requiring treatment: superior eyelid, inferior eyelid, and inner or external canthus. Simplifying, we can distinguish: (1) direct suture, (2) grafts, and (3) flaps.
Small defects can be directly sutured closed, even if they extend through the full thickness of the eyelid.
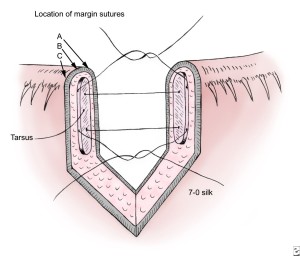 Pentagonal eyelid defect sutures directly with three margin sutures, to approximate eyelid lamellae.
Pentagonal eyelid defect sutures directly with three margin sutures, to approximate eyelid lamellae.
Repair of lower eyelid defects involving the eyelid margin and extending from one third to one half of the horizontal length of the eyelid margin requires advancement of adjacent tissue to effect closure.
Direct closure of full-thickness defects greater than one third of the eyelid may result in excessive tension in the wound, leading to wound dehiscence and eyelid notching. Larger defects may require complex reconstructions, involving transfer of adjacent tissues (“skin flaps”) or skin grafts from other parts of the face, body or eyelids.
We can classify skin grafts according to their thickness. The most frequently used graft is the Wolfe-Krause graft (0.80–1.00 mm), taken from the skin with a scalpel. Other grafts are the thin-skin grafts, such as the Ollier-Thiersh graft (0.20–0.35 mm), and the middle-thickness grafts such as the Blair-Brown (0.40–0.60 mm) or Padgett (0.60–0.80 mm) grafts. Both thin-skin and middle-thickness skin grafts can only be taken with the use of a dermatome.
By definition, a skin flap differs from a skin graft because it consists not only of skin but also of subcutaneous tissue with its subdermal plexus of vessels. Although it is completely raised from the underlying tissue, it is still connected by at least one side to the surrounding skin and fat. It is because of the vessels contained in this pedicle of the skin flap such that the flap can preserve its own blood supply, independent of the site on which it is placed.
Tenzel Semicircular Rotation Flap
The Tenzel semicircular advancement rotation flap is used to repair eyelid defects of moderate size. This technique involves the rotation of a semicircular musculocutaneous flap beginning at the lateral canthus, extending upward in a semicircular fashion. The flap is designed according to the size and location of the lower eyelid defect, and it must extend above the lateral canthal angle to ensure elevation of the lower eyelid during wound healing. Once the flap is rotated into position and sutured, adequate lateral canthal fixation must be achieved. Conjunctiva from the inferior fornix should be advanced or rotated into position to cover the posterior surface of the skin muscle flap. Skin closure of the semicircular donor site is the final step.
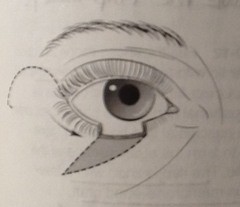 Tenzel Semicircular rotation advancement flap for lower eyelid defects.
Tenzel Semicircular rotation advancement flap for lower eyelid defects.
Tarsoconjunctival bridge flap (modified Hughes Flap procedure)
Lower eyelid defects greater than 50% of the horizontal length of the eyelid may be repaired with a tarsoconjunctival bridge flap from the upper eyelid. The modified Hughes procedure is performed as follows. A 4-0 silk traction suture is placed in the upper eyelid margin. The upper eyelid is everted over a Desmarres retractor. Tarsus and conjunctiva of the upper eyelid are incised horizontally 4 mm proximal to the eyelid margin. At least 4 mm of tarsus must be left for lid stability and to prevent the complication of upper lid entropion. A tarsal conjunctival flap is developed by dissecting the tarsus and conjunctiva away from the levator aponeurosis and Müller muscle. Dissection continues superior to the level of the Whitnall ligament.
The bridge flap is advanced into the defect of the lower eyelid; it may be moved laterally or medially, depending on the location of the lower eyelid defect. Edges of the tarsoconjunctival advancement flap are sutured to the remnants of the medial and lateral tarsus of the lower eyelid. If the lower eyelid defect involves either the medial or lateral canthal angle, the tarsoconjunctival flap must be fixated appropriately either to the lateral orbital tubercle or to the posterior lacrimal crest.
After the flap has been secured in position, a full-thickness skin graft is placed over the anterior surface. Skin can be harvested from the upper eyelid or from the retroauricular area. Alternatively, a locally based random flap may be advanced over the posterior lamella to create the new anterior lamella. The flap is separated at 4-6 weeks. A grooved director is slid underneath the flap anterior to the cornea, and the flap is divided. Conjunctiva is sutured to the lower eyelid margin. The Müller muscle and the levator aponeurosis are dissected away from the overlaying skin and allowed to retract. This prevents postoperative upper eyelid retraction and lagophthalmos.
Cutler Beard Flap & Reverse Cutler Beard Flap
The Cutler-Beard procedure is indicated for large central defects of the upper eyelid, while the Reverse Cutler beard Flap procedure is reserved for large central defects of the lower eyelid. This technique uses a full-thickness segment of the other eyelid tissue that is passed under an intact bridge of the eyelid margin. A full-thickness eyelid flap is sutured into the defect in the opposite eyelid. As with the flap created in a modified Hughes tarsoconjunctival procedure, the Cutler-Beard flap occludes vision for 6-8 weeks and must be divided in a second stage of the surgical procedure. It, therefore, is not suited for patients sighted only in the involved eye or of amblyogenic age. A modified Cutler-Beard procedure has been recently described by Yoon and .
Mustarde cheek rotation flap
Lower eyelid defects involving the entire lower eyelid may be reconstructed using a Mustarde cheek rotation flap. This large skin muscle flap is rotated from the cheek to repair large lower eyelid defects. Incision begins at the lateral canthal angle, extends upward onto the temple, and swings posteriorly just anterior to the ear and then inferiorly across the mandible. Establishing good vertical height to this flap is important so the correct position of the lateral canthal angle can be achieved postoperatively. The posterior lamella of this flap must be reconstructed with a free tarsoconjunctival graft, a nasal septal cartilage graft, or with mucous membrane.
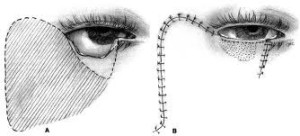 Mustarde’s Cheek Rotation Flap, to repair a large lower eyelid defect, post eyelid cancer removal
Mustarde’s Cheek Rotation Flap, to repair a large lower eyelid defect, post eyelid cancer removal