Orbital Lymphoma
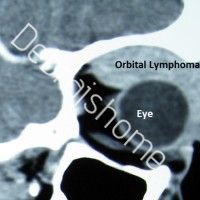
CT scan image showing orbital lymphoma
General Overview:
Orbital Lymphoma is a common type of Non-Hodgkin lymphoma which occurs near or behind the eye. Primary lymphoma of the orbit is amongst the most common orbital tumors & accounts for more than 50% of malignancies associated with the eye.
Adnexal and Orbital Lymphoma is associated with systemic lymphoma in 1/3rd of the cases.
Epidemiology:
Orbital lymphoma is more prevalent in Europe and Asia than in the United States.
Incidence of Orbital lymphoma increases as the age advances. This type typically is seen to affect elderly individuals; most likely in the age group of 70 years.
Female preponderance is noted in case of Orbital lymphoma. Females are most likely to get affected compared to males.
Clinical Presentation:
Orbital and ocular adnexal lymphoma has a gradual insidious onset and may progress slowly for over a year, before producing symptoms. The symptoms are usually secondary to pressure effects on the eye and surrounding ocular structures.
Clinical features include-
- Painless proptosis (bulging eyes), with or without motility disturbances
- Ptosis (drooping of eyelids)
- Double vision (diplopia) and
- Rarely, decreased vision
The lesions can be unilateral or bilateral.
Lymphomatous lesions can involve the preseptal portion of the eyelid.
Orbital lymphomas usually present with lesions most likely in the anterior superior orbit.
Consistency-The mass is usually rubbery to firm on palpation, with no palpable bony destruction.
The lacrimal gland, lacrimal sac, and extraocular muscles can also be similarly involved.
Orbital lymphoma can also occur in immunosuppressive patients eg. AIDS patients.
Conjunctival lymphoma has a characteristic salmon-pink appearance. It may be an extension of orbital or intraocular lymphoma.
Only 25% of the patients present with conjunctival involvement. Rest of the cases (75%) do not present with conjunctival involvement.
Pathology:
Orbital lymphoma is a B-cell non-Hodgkin lymphoma, and in most cases arises from mucosa-associated lymphoid tissue i.e orbital adnexal MALT lymphoma (OAML).
Laboratory Studies:
Laboratory studies are required to address the differential diagnosis of primary central nervous system lymphoma with ocular involvement (PCNSLO) and orbital lymphoma. They include the following:
- Complete blood count (CBC) with differential
- Erythrocyte sedimentation rate (ESR)
- Serum immunoprotein electrophoresis
- Rapid plasma reagin (RPR) screening
- Toxoplasmatiters
- Fluorescent treponemal antibody absorption (FTA-Abs) test
- Rheumatoid factor
- Antinuclear antibodies (ANA) test
- Angiotensin-converting enzyme (ACE)
- Cytomegalovirus (CMV) titers
A tuberculosis skin test is advisable. The serum lactate dehydrogenase (LDH) level is a prognostic indicator, with higher levels being indicative of a poorer prognosis.
Enzyme-linked immunosorbent assay (ELISA) for HIV is also recommended.
Imaging Studies:
- CT scan of Orbits-a sensitive radiological investigation, which helps in diagnosis of Orbital lymphoma. On CT scan of the orbits, orbital lymphomas are seen as well-defined, lobulated or nodular, homogeneous masses of relatively high density, with sharp margins. The lesions mould themselves to preexisting structures without eroding the underlying bone.
- Other tests include: Lumbar puncture, which is indicated to obtain cerebrospinal fluid (CSF), for cytology if the patient is believed to have CNS lymphoma.
- Bone marrow aspiration is used for staging systemic lymphomas.
- CT scans of the chest and abdomen are obtained to rule out retroperitoneal lymphoma.
- Bone scans may also be useful.
Biopsy:
Biopsy of the affected part of the lesion is sufficient to confirm diagnosis & also helpful in grading the tumor. Orbital Lymphoma is biopsied via orbitotomy surgery.
Treatment:
The recommended therapy is radiotherapy, whereas disseminated disease is treated with chemotherapy.
Lymphoid tumors of the conjunctiva have traditionally been treated with local radiation therapy. Some cases of conjunctival lymphoma were seen to spontaneously regress after biopsy; hence, follow-up without radiation has been considered an option for patients with mucosa-associated lymphoid tissue (MALT) lymphoma of conjunctival origin after the pathologic diagnosis by biopsy. Cryotherapy for certain conjunctival lymphomatous tumors has been suggested because of fewer ocular and systemic complications and lower cost.
Radiotherapy alone is a highly effective modality in the curative management of primary orbital lymphoma. Bilateral orbital disease itself, in the absence of systemic disease, is not an indication for chemotherapy.
Approximately 50% of orbital lymphomas are confined to the orbit at the time of diagnosis. In such cases, where there is no evidence of systemic lymphoma, local orbital low-dose (1500-3000 cGy) irradiation in fractionated doses is advised. High-grade tumors may require up to 4000 cGy. Appropriate shielding of the globe (lens-sparing technique) is recommended to minimize ocular complications of radiotherapy.
In cases of massive orbital involvement, both chemotherapy and radiation therapy can be simultaneously given.
Because secondary orbital lymphomas often exhibit widespread systemic involvement and usually have a more aggressive histologic classification than primary orbital lymphomas do, treatment of these lesions with systemic chemotherapy or systemic immunotherapy is warranted. In some cases, combining such systemic therapy with local radiation treatment is beneficial. After radiotherapy, local control may be achieved in 97-100% of patients.
Lymphomas respond well to monoclonal antibody (mAb) therapy, and research is ongoing to determine if such therapy can replace chemotherapy. Rituximab, ibritumomab, and epratuzumab are examples of mAbs that either are already in use or are being tested for use in lymphoma treatment. Intravenous rituximab has been used to treat low-grade lymphoma, with good results.
Antiangiogenic drugs, such as thalidomide, are also being researched for use in lymphoma treatment, as they are shown to slow the growth of cancer cells.
To read more on research performed by Dr. Debraj Shome in developing newer modalities of treatment for orbital lymphoma, click here:
http://www.ncbi.nlm.nih.gov/pubmed/18772675
http://www.ncbi.nlm.nih.gov/pubmed/22737325
Proptosis Surgery | Big Eyes | Cavernous Hemangioma | Orbital Lymphoma | Oculoplastic Surgery India
Exophthalmos, also called proptosis, is a bulging of the eye anteriorly out of the orbit (bulging eyes or big eyes). Exophthalmos can be either bilateral (as is often seen in Graves’ disease or Thyroi…